Elizabeth Dzeng's research shows doctors' moral distress surrounding futile end of life treatments.
Doctors' words - ‘torture’, ‘gruesome’, ‘abuse’, ‘mutilate’ and ‘cruel’ evoke images more fitting of penal regimes than hospitals. The moral toll exacted upon these physicians is evident in descriptions such as feeling ‘violated’ and ‘traumatised’.
Elizabeth Dzeng
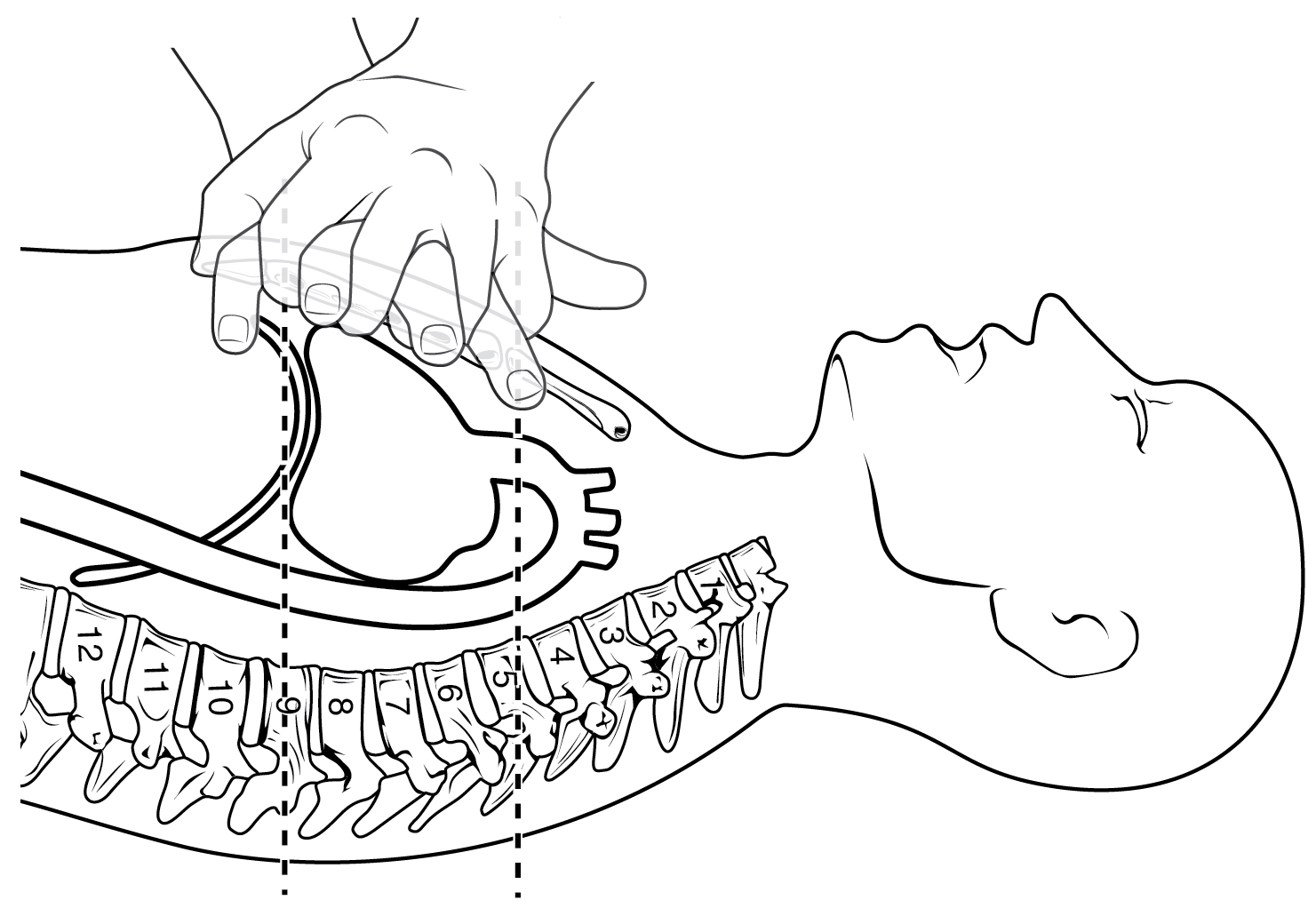
Trainee doctors think they are being asked to prolong some patients’ lives unnecessarily and describe such cases as being tantamount to torture and abuse, according to a new study.
The research, led by Elizabeth Dzeng, a Gates Cambridge Scholar at the University of Cambridge, is the first to focus on US doctors’ moral distress surrounding resuscitation and treatments that they believe may be futile at the end of life and has implications for the UK as more power is handed from doctors to patients’ representatives around end of life issues.
The qualitative study, titled "Moral Distress Amongst American Physician Trainees Regarding Futile Treatments at the End of Life: A Qualitative Inquiry", is published in the Journal of General Internal Medicine.
Elizabeth conducted in-depth interviews with 22 physician trainees in internal medicine at three accredited medical centres in the US and asked how they reacted and responded to ethical challenges arising in the context of perceived futile treatments at the end of life and how they felt about its ethical implications.
It found that doctors who are required to perform procedures such as resuscitation which they feel are futile or harmful have significant moral qualms that they are prolonging suffering as opposed to providing care. Some cope with these by developing detached and dehumanising attitudes towards patients.
One said of a patient: “It felt horrible, like I was torturing him. He was telling us we were torturing him. I did not think we were doing the right things.”
Another said: “I agree with giving the patient’s choice, but oftentimes it’s the family member. If the patient says, “Torture me, I want everything done.” Fine. The family member is doing it for other reasons. Like guilt; they can’t let go.”
Ways of coping ranged from formal and informal conversations with colleagues and superiors about the emotional and ethical challenges of providing care at the end of life to a tendency among some to dehumanise the patient.
One trainee said: “We’re abusing a body and I get that, but as long as I remember I’m only abusing a body and not a person, it’s okay. Frequently when it’s an inappropriate code, that’s what’s happening.”
Trainees also said that the hierarchical nature of their relationship with other doctors meant they felt powerless to have any influence on decisions.
Dzeng [2011] is completing a PhD on medical sociology and ethics and is also a fellow in General Internal Medicine at the Johns Hopkins School of Medicine. She said: “Our study sheds light on a significant cause of moral distress amongst physician trainees when they feel obligated to provide treatments at the end of life that they believe to be futile or harmful. Their words – ‘torture’, ‘gruesome’, ‘abuse’, ‘mutilate’ and ‘cruel’ evoke images more fitting of penal regimes than hospitals. The moral toll exacted upon these physicians is evident in descriptions such as feeling ‘violated’ and ‘traumatised’. Previous research shows that moral distress can have significant negative effects on job satisfaction, psychological and physical well-being and self-image, resulting in burnout and thoughts of quitting.”
The paper is part of a larger study investigating the influence of institutional cultures and policies on physicians' and trainees' views on resuscitation orders. A previous paper found that in hospitals with cultures and policies which prioritised patient autonomy over the patients' best interest, physicians tended to give patients a menu of choices without guidance or recommendations over whether resuscitation would be beneficial or merely prolong suffering. It explored the effect of moves towards greater patient autonomy over end of life decisions. Although this was an understandable reaction to the paternalistic approach often adopted by doctors in the past, the paper voiced fears that the pendulum may have swung too far, to the detriment of patients themselves.
Picture credit: Cardio-pulmonary resuscitation courtesty of Wikimedia.